The rising cost of living has become a significant public health concern, particularly for low-income individuals who are struggling daily to survive. Addressing the social determinants of health among this population remains an urgent issue, as many face ongoing challenges accessing essential needs such as food, housing, transportation, and healthcare. During my assessment of some of the low-income individuals, I found that several individuals eat only once a day to save money for rent. Many reported choosing to go hungry rather than risk homelessness. Some have been living in their cars for nearly a year, while others rely on the homes of friends to shower and change clothes. It is heartbreaking to witness the difficult situations people endure every day to stay alive.
The rising cost of living has multiple impacts on health and well-being. According to Grewal et al. (2024), increasing housing costs—one of the key components of living expenses—can have both direct and indirect health consequences. Their study indicates that:
- Financial strain from high housing and living expenses contributes to increased stress, anxiety, and depression, particularly among renters and low-income individuals.
- Food insecurity often results when households must prioritize rent or transportation over nutrition, leading to poor dietary intake and higher risks of chronic diseases.
- Limited access to healthcare arises when individuals cannot afford medical visits, medications, or preventive care due to competing financial demands.
- Housing instability or homelessness can expose individuals to unsafe environments, lack of sanitation, and interrupted social support networks, which worsen both physical and mental health outcomes.
Overall, Grewal et al. (2024) emphasize that the effects of rising housing and living costs are unequally distributed, disproportionately affecting low-income individuals who already face multiple barriers to health. This highlights the need for comprehensive policy approaches that integrate housing affordability, income support, and healthcare access as essential strategies to promote health equity.
Source: https://doi.org/10.1186/s12889-024-18360-w
 Contributing factors to the High Obesity Rates Among African American Women
Contributing factors to the High Obesity Rates Among African American WomenResearch reports that American women are disproportionately affected, with the highest obesity rates among all groups in the U.S. About 80% are classified as overweight or obese.
Disparities in weight loss
Research indicates that African American (AA) women tend to lose less weight compared to their Caucasian counterparts.
Contributing Factors
The contributing factors to the disparities are;
- Limited access to nutritious food
- Inadequate health insurance
- Lack of safe spaces for physical activity
Barriers to Weight Management
Challenges that hinder weight management efforts include:
- Personal beliefs
- Limited time
- Family dynamics
- Lack of motivation
- Financial constraints
Cultural Influence on Body Image
Cultural norms within the AA community, which often embrace larger body sizes and promote a positive body image, can also influence health behaviors. While fostering a positive body image has psychological benefits, it may reduce motivation to maintain a healthy weight. In Black culture, obesity and being overweight are often considered acceptable and carry little to no stigma. Cultural perspective may partially explain why general health promotion efforts are less effective in this community. The study reports that many Black female students aim to embody the culturally valued “thick and curvy” figure, consuming specific foods to shape their bodies while avoiding activities that might result in weight loss.
Why it may be difficult to seek care
A deep-rooted distrust of the healthcare system makes it difficult for many AA women to seek medical advice or treatment.
Physical inactivity as a health risk factor
Underestimating body weight can reduce engagement in healthy behaviors, such as regular physical activity. Physical inactivity is a major contributor to non-communicable diseases and mortality, emphasizing the need to address these issues within the AA community.
 Four lifestyle changes to reduce the development of Uterine Fibroids (UFs)
Four lifestyle changes to reduce the development of Uterine Fibroids (UFs)Uterine fibroids (UFs) are the most common benign tumors found in women of reproductive age, with a disproportionate impact on women of color. These disparities are believed to be combined with environmental, genetic, and socio-economic factors.
Some of the lifestyle changes that can help prevent or reduce the development of uterine fibroids are;
- Decreasing Alcohol consumption: It’s advised that women decrease their alcohol consumption to reduce the risk of developing uterine fibroids (UFs). Studies have reported an association between alcohol intake and an increased likelihood of UFs. Studies believe that alcohol may alter hormone levels and disrupt hormonal balance, contributing to the formation of UFs. It is advisable to consult with a healthcare professional for personalized advice based on unique health occurrences. By being mindful of alcohol consumption and adhering to recommended limits, proactive steps can be taken to lower the risk of UFs.
- Engage in at least four hours of vigorous physical activity per week: Research has found a significant association between an increased BMI and the risk of UFs. Obesity is believed to be a contributing factor to UF. Studies believe that women who engage in at least four hours of vigorous physical activity per week are more likely to encounter a decrease in the risk factors of UFs.
- Consuming more fruits, Vegetables, and dietary fibers: High intake of processed and refined foods, unhealthy fats, and sugary drinks, and low consumption of fruits, vegetables, and fiber-rich foods may contribute to hormonal imbalances, inflammation and oxidative stress, thereby encouraging the growth of UFs as indicated in the research. Additionally, a lack of fruits, vegetables, and fiber-rich foods has been reported to be associated with an elevated risk of UFs. Fruits, vegetables, and fiber-rich food are excellent sources of antioxidants, vitamins, and minerals that help combat oxidative stress and inflammation. Specifically, Dietary fiber has been indicated to have protective impacts against UFs by supporting hormonal balance and improving regular bowel movements. Hence, adopting a healthy and balanced diet with whole grains, fruits, vegetables, lean proteins, and healthy fats is essential.
- Managing stress: Studies have found that chronic psychological stress could increase the risk of uterine fibroids and indicated a significant link between chronic psychological stress and an elevated risk of UFs, predominantly among non-Hispanic Black women. Eating healthy, exercising regularly, getting enough sleep, relaxing, connecting with friends and family, and practicing mindfulness are some ways to manage stress.
 Should we throw away our medicines after the ‘Best Before’ or Expiry date?
Should we throw away our medicines after the ‘Best Before’ or Expiry date?Introduction
One of man’s best inventions is drugs, especially disease-specific ones. Drugs are substances other than food, which can prevent, relieve the symptoms, or cure an abnormality or disease. Globally, the cost of drugs has soared over the years, resulting in a situation whereby low-income earners are unable to buy branded medications. In underdeveloped and developing countries where food and drug agencies have poor capacity to perform their regulatory functions optimally, we tend to see the proliferation of substandard or fake drugs. So many times, this ugly trend is energized by not just greed but by the market demands for affordable medications.
Why Medication exceeds expiry date
To mitigate the challenge of not being able to buy drugs, when necessary, people from resource-limited settings stack up some essential medications in their homes, which eventually exceed the best before or expiry dates on them. Sometimes, doctors could change a patient’s prescription because of reactions, allergies, or inability to purchase the drug, which could result in leftover drugs that eventually exceed the expiration date. Also, big pharmacies and patent-drug stores cannot sell all their stock, leading to the expiration of some drugs. This situation has raised many questions about the safety of these drugs after their expiration or beyond the “best before” date. Because of the importance of drugs and the health risks involved when taken wrongly, people have always consciously discarded unused drugs when it’s past the expiration date, even one day.
How Safe is a drug after the expiry date?
The debate about drugs being safe after their expiration date has persisted over the years, as many people still hold the opinion that pharmaceutical companies deliberately label their drugs with short shelf lives to guarantee steady patronage. Eventually, most of these unused drugs are discarded. The context that drugs can still be safe for a long time after expiration has gained several affirmations. In a recent study by Benjamin Davido and others titled ‘Efficacy of Expired Antibiotics: A Real Debate in the Context of Repeated Drug Shortages’ published in MDPI Journal “Antibiotics”, it was reported that when appropriately stored in line with the expected conditions, no expired antibiotics tested failed to be potent after one year of expiration. In another study by Sushil Sharma and others, titled ‘A study to investigate the chemical potency, physical stability, and efficacy of analgesic agents over a period of two years post their expiry date’ published in the “Medical Journal Armed Forces India”, it was seen that drugs such as Diclofenac, Piroxicam, and Ibuprofen retained their stability, analgesic efficacy, chemical active ingredients and by implication their potency up to a duration of two years after expiration.
Important factors to consider
However, the issues of proper storage and handling can play a big role, especially in the tropical climate of West Africa and other geographical regions. Hence, people in the tropics may have to rely on their capacity to store their drugs in the required condition in deciding whether to use a drug past the expiration date or not.
Conclusion
This article doesn’t advocate for the use of expired medication but to reduce anxiety about accidental use. It is essential to understand factors that impact drug stability.
(Written by Ebenezer Dic-Ijiewere PhD.)
NB: Always consult your healthcare professionals regarding expired medications to ensure medication safety and effectiveness.
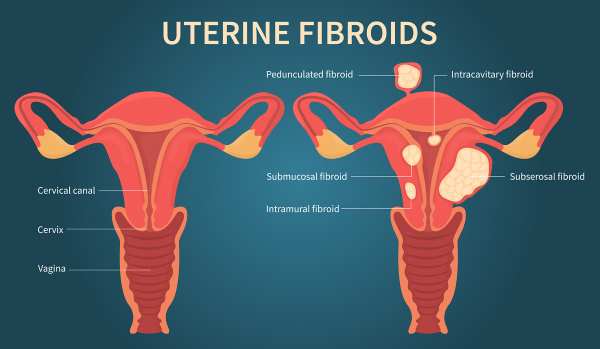 Risk Factors for Uterine Fibroids Among Black Women
Risk Factors for Uterine Fibroids Among Black WomenUterine fibroids (UFs) represent the most prevalent non-cancerous tumors among women of reproductive age. Symptomatic fibroids can lead to significant health issues and are the primary reason for hysterectomies in the United States and globally, contributing to substantial socioeconomic impacts and affecting over 70% of women of reproductive age (Langton et al., 2024). African American women tend to develop fibroids approximately 10 years earlier than White women in the US and bear a disproportionate health burden from these tumors
Black women experience UFs at higher rates, with an earlier onset, more severe symptoms, and faster disease progression compared to other groups.
According to Sithembinkosi Ndebele (2024), 85% of participants were non-Hispanic Blacks. Black participants had a higher likelihood of a UF diagnosis, and the following risk factors were reported contributing to the high prevalence of UFs in Black individuals:
- Socioeconomic Status: Lower socioeconomic status is reported to increase the rates of UFs.
- Adverse Environmental Exposures: Increased exposure to environmental pollutants is associated with a higher prevalence of UFs.
- Chronic Stress: Experiences that increase chronic stress are significant contributors.
Lifestyle and socioeconomic factors, closely tied to neighborhood characteristics, further influence UF prevalence. These factors include:
- Body Mass Index (BMI): A higher BMI correlates with a higher risk of UFs.
- Alcohol Use: Regular alcohol consumption is positively correlated with UF diagnosis.
- Income and Occupation: These factors influence access to healthy food and healthcare.
 Key Strategies to Cope with Stress
Key Strategies to Cope with StressStress has a significant impact on overall health, playing a crucial role in the development of various diseases and placing a substantial strain on the healthcare system (Shchaslyvyi et al., 2024). It is closely linked to numerous long-term health problems, especially cardiovascular conditions, which are often worsened by daily psychosocial pressures like job-related stress (Shchaslyvyi et al.,2024) It is essential to understand the healthy ways to cope with or manage stress.
Various strategies recommended according to the CDC (2025)
- Take Care of Your Mind
Limit news and social media exposure: Excessive exposure to harmful or distressing news can exacerbate stress.
Make time to unwind: Incorporate relaxation practices such as deep breathing, stretching, or meditation.
Keep a journal: Writing can help you process emotions, reflect on your thoughts, and release tension.
Spend time outdoors: Whether you are being active (walking, hiking) or just relaxing outside, nature can be a calming presence.
Practice gratitude: Regularly noting things you are grateful for helps improve emotional well-being.
Connect with others: Talking to trusted friends, family, or community/faith-based groups provides support.
- Take Care of Your Body
Get enough sleep: The CDC recommends 7 hours or more per night for adults and suggests maintaining a consistent sleep schedule.
Move more: Physical activity is one of the most effective ways to reduce stress; even small amounts can help.
Eat well: A balanced diet (fruits, vegetables, lean proteins, whole grains, low-fat dairy) supports both physical and mental health.
Limit alcohol and avoid substance misuse: Moderating alcohol intake, avoiding illegal drugs, and not misusing prescription medication are essential.
Avoid tobacco: Smoking, vaping, and the use of other tobacco products can worsen stress or its effects.
Stay up to date with healthcare: Regular check-ups, screenings, and vaccinations help you maintain your physical health — which can help buffer stress.
- Integrate Physical and Mental Health
The CDC emphasizes that mental well-being and physical health are closely linked. Regular physical activity is not only good for the body but also supports emotional resilience.
It encourages finding a “right combination” of coping techniques that work for you — not everyone copes the same way.
- Know When to Seek Extra Support
The CDC notes that while stress is everyday, chronic stress (long-term) can lead to serious health problems.
If you’re struggling to cope or stress is affecting your daily life, it’s okay to reach out for help. They list resources, including crisis lines.
Sources
CDC. (2025)
International Journal of Environmental Research and Public Health, 21(8), 1077–1077. https://doi.org/10.3390/ijerph21081077
 How to Decrease High Cholesterol Levels
How to Decrease High Cholesterol LevelsHigh cholesterol (hypercholesterolemia) refers to elevated levels of cholesterol in the blood, especially low-density lipoprotein cholesterol (LDL-C)—which is widely regarded as a key modifiable risk factor for atherosclerosis and cardiovascular disease (CVD). LDL-C can deposit in arterial walls, forming plaques that narrow arteries and increase the risk of heart attack and stroke. Meanwhile, high-density lipoprotein (HDL-C) is considered “good” cholesterol because it helps transport cholesterol away from the arteries to the liver for excretion. Several factors can increase the level of cholesterol in the blood, as indicated below
Factors That Contribute to Elevated Cholesterol
- Poor diet
- Lack of Physical Exercise
- Excess body weight
- Smoking increases cholesterol profile, and excessive alcohol increases triglycerides
- Genetic traits
- Chronic stress and poor sleep
- Diet low fiber
To decrease high cholesterol in the blood, it is important to make positive changes to health behaviors by following the strategies below:
Strategies to Decrease High Cholesterol Levels
- Reduce intake of saturated and trans fats, and substitute with MUFA and PUFA-rich foods such as fatty fish(Salmon and Mackerel), olive oil/canola oil, Avocado/nuts
A study by Okobi et al. (2023) found that an avocado-rich diet can lower total cholesterol (TC) and low-density lipoprotein (LDL) levels.
- Increase consumption of food high in soluble fiber, such as oats, fruits, apples, and legumes.
- Regular aerobic exercise for 150 minutes/week lowers LDL and triglycerides and improves HDL.
- Losing excessive weight will improve LDL profiles.
- Quitting smoking will improve cardiovascular health and HDL levels


