Sleep is essential for the health and well-being of children, adolescents, and adults. Quality sleep supports emotional well-being, metabolic health, cognitive function, mental health, and cardiovascular and cerebrovascular health. Additionally, getting sufficient, high-quality sleep helps reduce the risk of fatigue-related accidents and injuries, such as motor vehicle accidents and workplace incidents.
Recommended Sleep Duration
The American Academy of Sleep Medicine (AASM) and the Sleep Research Society (SRS) recommend that adults aim for at least 7 hours of sleep each night to promote optimal health. Similarly, the National Sleep Foundation (NSF) advises adults to get 7 to 9 hours of sleep per night, with older adults requiring 7 to 8 hours.
Prevalence of Sleep Disorders and Mental Health Impacts
About one-third of the population experiences insomnia symptoms, such as difficulty falling or staying asleep. Additionally, 4% to 26% of individuals report excessive sleepiness, and 2% to 4% have obstructive sleep apnea. Insomnia is associated with a significantly increased likelihood of mental health issues; individuals with insomnia are 10 times more likely to experience clinically significant depression and 17 times more likely to experience anxiety compared to those without insomnia. Poor sleep is also linked to post-traumatic stress, eating disorders, and psychosis spectrum experiences, such as delusions and hallucinations.
Improving sleep Quality
Improving sleep quality benefits mental health, and research reports that sleep plays a causal role in mental health challenges. Better sleep positively affects future mental health, even those without clinical symptoms.
Strategies for Improving Sleep Quality
- Creating a relaxing sleep environment
- Limiting daytime naps
- Managing stress and worries
- Being mindful of food and drink choices
- Sticking to a consistent sleep schedule
- Incorporating physical activity into daily routines.
 Risk Factors for Uterine Fibroids Among Black Women
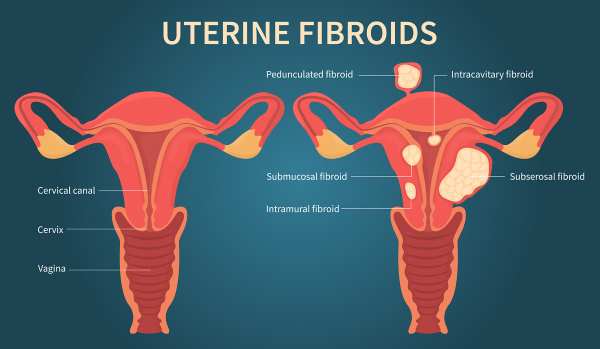
Risk Factors for Uterine Fibroids Among Black WomenUterine fibroids (UFs) represent the most prevalent non-cancerous tumors among women of reproductive age. Symptomatic fibroids can lead to significant health issues and are the primary reason for hysterectomies in the United States and globally, contributing to substantial socioeconomic impacts and affecting over 70% of women of reproductive age (Langton et al., 2024). African American women tend to develop fibroids approximately 10 years earlier than White women in the US and bear a disproportionate health burden from these tumors
Black women experience UFs at higher rates, with an earlier onset, more severe symptoms, and faster disease progression compared to other groups.
According to Sithembinkosi Ndebele (2024), 85% of participants were non-Hispanic Blacks. Black participants had a higher likelihood of a UF diagnosis, and the following risk factors were reported contributing to the high prevalence of UFs in Black individuals:
- Socioeconomic Status: Lower socioeconomic status is reported to increase the rates of UFs.
- Adverse Environmental Exposures: Increased exposure to environmental pollutants is associated with a higher prevalence of UFs.
- Chronic Stress: Experiences that increase chronic stress are significant contributors.
Lifestyle and socioeconomic factors, closely tied to neighborhood characteristics, further influence UF prevalence. These factors include:
- Body Mass Index (BMI): A higher BMI correlates with a higher risk of UFs.
- Alcohol Use: Regular alcohol consumption is positively correlated with UF diagnosis.
- Income and Occupation: These factors influence access to healthy food and healthcare.
 Should we throw away our medicines after the ‘Best Before’ or Expiry date?
Should we throw away our medicines after the ‘Best Before’ or Expiry date?Introduction
One of man’s best inventions is drugs, especially disease-specific ones. Drugs are substances other than food, which can prevent, relieve the symptoms, or cure an abnormality or disease. Globally, the cost of drugs has soared over the years, resulting in a situation whereby low-income earners are unable to buy branded medications. In underdeveloped and developing countries where food and drug agencies have poor capacity to perform their regulatory functions optimally, we tend to see the proliferation of substandard or fake drugs. So many times, this ugly trend is energized by not just greed but by the market demands for affordable medications.
Why Medication exceeds expiry date
To mitigate the challenge of not being able to buy drugs, when necessary, people from resource-limited settings stack up some essential medications in their homes, which eventually exceed the best before or expiry dates on them. Sometimes, doctors could change a patient’s prescription because of reactions, allergies, or inability to purchase the drug, which could result in leftover drugs that eventually exceed the expiration date. Also, big pharmacies and patent-drug stores cannot sell all their stock, leading to the expiration of some drugs. This situation has raised many questions about the safety of these drugs after their expiration or beyond the “best before” date. Because of the importance of drugs and the health risks involved when taken wrongly, people have always consciously discarded unused drugs when it’s past the expiration date, even one day.
How Safe is a drug after the expiry date?
The debate about drugs being safe after their expiration date has persisted over the years, as many people still hold the opinion that pharmaceutical companies deliberately label their drugs with short shelf lives to guarantee steady patronage. Eventually, most of these unused drugs are discarded. The context that drugs can still be safe for a long time after expiration has gained several affirmations. In a recent study by Benjamin Davido and others titled ‘Efficacy of Expired Antibiotics: A Real Debate in the Context of Repeated Drug Shortages’ published in MDPI Journal “Antibiotics”, it was reported that when appropriately stored in line with the expected conditions, no expired antibiotics tested failed to be potent after one year of expiration. In another study by Sushil Sharma and others, titled ‘A study to investigate the chemical potency, physical stability, and efficacy of analgesic agents over a period of two years post their expiry date’ published in the “Medical Journal Armed Forces India”, it was seen that drugs such as Diclofenac, Piroxicam, and Ibuprofen retained their stability, analgesic efficacy, chemical active ingredients and by implication their potency up to a duration of two years after expiration.
Important factors to consider
However, the issues of proper storage and handling can play a big role, especially in the tropical climate of West Africa and other geographical regions. Hence, people in the tropics may have to rely on their capacity to store their drugs in the required condition in deciding whether to use a drug past the expiration date or not.
Conclusion
This article doesn’t advocate for the use of expired medication but to reduce anxiety about accidental use. It is essential to understand factors that impact drug stability.
(Written by Ebenezer Dic-Ijiewere PhD.)
NB: Always consult your healthcare professionals regarding expired medications to ensure medication safety and effectiveness.
 Unlocking the Benefits of Consistent Physical Activity
Unlocking the Benefits of Consistent Physical ActivityInadequate exercise or physical activity can contribute to the prevalence of non-communicable diseases. Given that non-communicable diseases account for over 80% of deaths in some nations, they are regarded as “the number one killer” globally. Physical exercise is any movement that requires energy, like housework, manual labor, walking, or manual labor. Exercise, on the other hand, is a regimen of physical activity that is organized and planned to enhance physical fitness.
Evidenced-based benefits.
- Physical Health: Research reported that 150 min of moderate-intensity or 75 min of vigorous-intensity physical activity led to a 14% risk reduction in all-cause mortality in patients with cardiovascular disease. In healthy adults, the risk decreased by 7%. Regular exercise has been shown in numerous studies to be beneficial in lowering the risk of cardiovascular disease as well as improving the health of patients with a variety of other conditions, such as certain cancers. stroke, type 2 diabetes, age-related sarcopenia, obesity, and multiple sclerosis.
- Mental Health: Research findings indicate that youth with mild to moderate mental health issues can benefit from organized sports and exercise programs. In one study, participants highlighted the significance of intensity choice for their enjoyment and commitment to the program, and it was shown that a self-selected intensity sport and exercise intervention was beneficial for depression. Research findings indicate that youth with mild to moderate mental health issues can benefit from organized sports and exercise programs. In one study, participants highlighted the significance of intensity choice for their enjoyment and commitment to the program, and it was shown that a self-selected intensity sport and exercise intervention was beneficial for depression. Also, engaging in physical exercise for 14 weeks can considerably improve mental symptoms, reduce anxiety and somatization, lessen obsessive-compulsive symptoms, and lift depressed moods.
- Quality Sleep: Study indicated that quality of sleep was positively impacted by exercise. Additionally, insomnia was somewhat alleviated following the exercise intervention. For instance, studies reveal that first-year students who exercise more get better sleep than those who exercise less during the night.
Evidenced-based research recommended the following:
- Adults should aim for more than 300 minutes of moderate-intensity aerobic physical activity, 150 minutes of vigorous-intensity aerobic physical activity spread out over the week, or an equivalent mix of moderate-intensity and vigorous-intensity aerobic physical activity.
- Engage in moderate-to-intense muscle-strengthening activities that target all major muscle groups two or more days a week.
- Adults 65 and older engage in multicomponent physical activity that involves functional balance and strength training at a moderate or higher intensity for at least three days a week in addition to aerobic exercises.
 The Health Effects of Stress
The Health Effects of StressOverview of Stress: Stress significantly affects health, contributing to disease development and burdening healthcare systems considerably. It is a significant factor in various ongoing health issues, particularly cardiovascular diseases, which are often impaired by everyday psychosocial pressures, such as work-related stress.
The following are the roles of stress in disease development.
Gender Differences in Stress Responses: Gender plays a vital role in how individuals experience and manage stress. Research reports that women are more likely to develop mood disorders and autoimmune. At the same time, men tend to have higher rates of early substance abuse, infectious disease, mortality, and antisocial behavior. Unsuccessful stress management can lead to severe physical and mental health consequences for both individuals and communities.
Physiological Responses to Stress: The study reports that stressful events can trigger emotional responses such as anxiety and worry, impacting the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic-adrenal-medullary (SAM) system, which may lead to unhealthy lifestyle choices, comprising poor sleep, alcohol consumption, decreased physical activity and increased smoking thereby increase the risk of diseases.
Chronic Stress in Specific Environments: Chronic stress in educational settings and workplaces impacts mental and physical health noticeably. Also, it indicates that occupational stress significantly affects mental well-being.
Traumatic Events as a Stress Source: Traumatic events are a prevalent source of stress that affects a large portion of the population. The study reports that In North America, about 60% to 75% of individuals will experience a traumatic event in their lifetime, including serious accidents, exposure to war, sexual assault, chronic childhood abuse, or neglect.
 The Health Risk Hiding In Your Light Switch and How to Prevent It
The Health Risk Hiding In Your Light Switch and How to Prevent ItLight at night (LAN) refers to the use of artificial or natural light during nighttime hours for visibility purposes.
Deprato et al. (2025) reports that approximately 80% of the global population is exposed to light-polluted skies, and LAN is now considered a major environmental pollutant. Sources include streetlights, vehicles, homes, industries, and even atmospheric reflections.
LAN disrupts the body’s circadian rhythm, the internal 24-hour clock regulated by the brain’s suprachiasmatic nucleus. When artificial light interferes with natural dark–light patterns, it delays the circadian clock and sleep-wake cycle, leading to melatonin suppression, sleep disturbances, and an increased risk of various diseases (Deprato et al., 2025). Blue-rich and bright LED lights cause the most significant disruption (Deprato et al., 2025). The study reports that LAN exposure is linked to higher rates of depression, bipolar disorder, anxiety, and other severe mental disorders, likely due to circadian misalignment, sleep deprivation, and changes in brain chemicals such as serotonin and dopamine.
Implications:
1.The findings suggest that light pollution and artificial light exposure at night are not only environmental/visual concerns but also have mental health implications.
2. Encourages rethinking nighttime habits — including screen use before bed, bedroom lighting, blackout curtains, and managing exposure to streetlights or indoor lights at night.
3.The implications of light at night may vary by culture or by groups
4. Designing homes and neighborhoods that minimize intrusive nighttime lighting in bedrooms, promoting lighting standards that consider human health
Prevention/ Mitigation strategies
1.Reduce screen time before bed: Use “night mode” or blue-light filters on devices, dim the brightness, and avoid stimulating content.
2. Improve bedroom lighting: Use blackout curtains, turn off or dim indoor lights, remove bright electronic indicators, and opt for warm, low-intensity lighting in the evening.
3. Maintain a consistent sleep–wake schedule: Even if artificial light is present, a regular circadian rhythm helps mitigate disruptions.
4. Use lighting design for sleep: In the evening, switch to warmer (red/orange) wavelengths; avoid bright overhead white/blue light late at night.
5.Monitor and adjust ambient outdoor lighting: If streetlights are intrusive, consider using blackout curtains or an eye mask; if indoor lighting spills into the night, turn off non-essential lights.
Source: https://doi.org/10.1016/j.scitotenv.2025.179188
 Successful interventions for managing or reducing effects of Postpartum depression (PPD)
Successful interventions for managing or reducing effects of Postpartum depression (PPD)Postpartum depression (PPD) presents a significant public health concern, affecting not only the physical and mental well-being of mothers but also that of their infants. Research suggests that approximately 13 million women worldwide are diagnosed with PPD annually (Xu et al., 2023). Mild depressive symptoms are experienced by around 50% to 75% of mothers, with 10% to 15% developing postpartum depression within the first week after childbirth (Xu et al., 2023).
Understanding preventive measures to reduce its prevalence is very crucial.
1. Exercise intervention has proven effective in preventing PPD disorders. In a 12-week exercise intervention study, aerobic exercise was found to relieve postpartum depression symptoms in PPD patients. Engaging in suitable aerobic exercise during pregnancy has been reported to promote pelvic mobility and improve birth canal space to relieve maternal labor pain. However, it also aids in preventing pregnancy complications. Studies suggest that PPD symptoms may manifest during pregnancy, with a similar 12% occurrence rate of depression reported, which indicates that preventive measures during pregnancy may have a significant impact on reducing PPD (Xu et al., 2023).
Moreover, research indicates that the antidepressant effects of exercise can persist beyond the cessation of physical activity. Therefore, research suggested that incorporating aerobic exercise into prenatal care may substantially prevent PPD more than exercise as a postpartum treatment strategy.
Engaging in moderate exercise during pregnancy can reduce the likelihood of developing postpartum depression (PPD) among expectant mothers. Partaking in at least 150 minutes of moderate-intensity aerobic exercise per week significantly enhances the efficacy of physical activity in preventing and treating PPD (Xu et al., 2023). Moderate aerobic exercise prompts the release of endorphins, which uplift mood and alleviate symptoms of anxiety and depression. Additionally, it helps regulate hormone levels, improve sleep quality, and enhance self-awareness and self-esteem, thereby positively influencing the mitigation of postpartum depression (Xu et al., 2023).
Also, social support plays a vital role in maintaining the mental well-being of pregnant and postpartum women, with supervised exercise and team-based exercise serving as effective avenues for providing such support. For instance,
• Team exercise fosters a positive environment for maternal emotional communication, and sharing maternal emotions enhances mothers’ childbirth knowledge and skills, reduces fear of labor pains, alleviates negative emotions, improves interpersonal communication, and enhances self-efficacy (Xu et al., 2023).
• Supervised exercise, which involves physical activities piloted and supervised by healthcare professionals or fitness trainers, ensuring that exercises are safe and suitable for individual pregnant and postpartum women. Participating in supervised exercise classes or programs also offers opportunities for social interaction, which is critical for mental well-being and can lighten feelings of isolation by connecting with other new mothers and professionals in a supportive setting (Xu et al., 2023).
2. Music therapy, when used as an adjunct to conventional psychotherapies, has been shown to improve physiological symptoms and effectively reduce negative emotions without any adverse side effects. It can positively impact and alleviate symptoms of PPD, offering a safe and affordable substitute to standard treatments. Music therapy is considered to reduce the need for pharmacological interventions during PPD treatment. Research has indicated that music therapy interventions such as music listening, improvisation, songwriting, singing, relaxation and meditation, and lyric analysis effectively reduce the risk of prolonged PPD and it can encourage strengths, empower individuals, and foster connections with themselves and others (Patch & Short, 2022).
References
Xu, H., Liu, R., Wang, X., & Yang, J. (2023). Effectiveness of aerobic exercise in the prevention and treatment of postpartum depression: Meta-analysis and network meta-analysis. PLOS ONE, 18(11), e0287650–e0287650. https://doi.org/10.1371/journal.pone.0287650
Patch, M. C., & Short, A. E. (2022). Addressing the “Baby Blues”: Developing a Music Therapy Model for Prevention and Treatment of Postpartum Depression. Australian Journal of Music Therapy, 33(2), 82–90. https://eds.p.ebscohost.com/eds/pdfviewer/pdfviewer?vid=10&sid=e5bc3ad9-8160-4ed8-bb4f-752141ecd9c5%40redis



