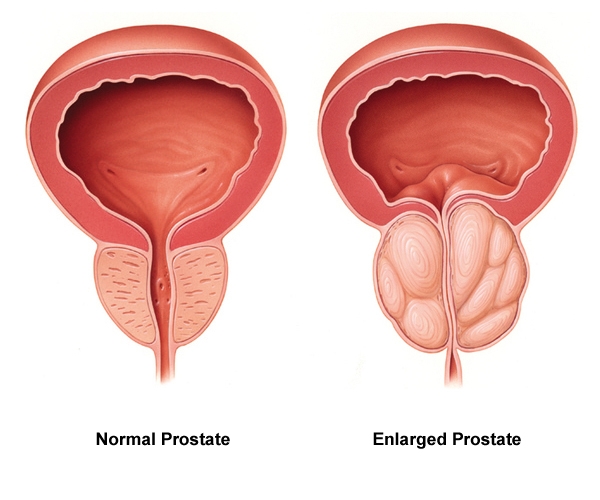
The prostate is a small, walnut-sized, shaped organ below the bladder and in front of the rectum. The main functions are to create fluids for semen and force semen through the urethra during ejaculation. It is usual for the prostate to get larger as one age. Because of the location just below the bladder and in front of the rectum, also wrapping around the upper part of the urethra, the tube that carries urine from the bladder out of the body, it means abnormal prostate conditions can affect urination and sexual function. The prostate is prone to three main conditions, which are Prostatitis, an infection or inflammation of the prostate gland; Benign prostatic hyperplasia (BPH), an aging-related enlargement of the prostate gland; Prostate cancer, the growth of cancerous cells inside the prostate, which may break out of the gland and affect other parts of the body.
Prostatitis
This is the inflammation (swelling) of the prostate gland, and common causes include infection (usually bacteria), injury, or an immune system disorder. The symptoms may include the inability to urinate, Painful or difficult urination, and painful ejaculation, accompanied by fever, Blood in the urine (hematuria), and Severe discomfort or pain in the pelvic area or genitals.
The Risk factors for prostatitis include:
Previous prostatitis, Infection of the urinary or reproductive system, HIV infection or AIDS, Use of a tube inserted into the urethra to drain the bladder (urinary catheter), and Diagnostic sampling of prostate tissue (biopsy).
Laboratory tests for Prostatitis include Urinalysis, urine microscopy/culture/sensitivity, HIV, measurement of Prostatic specific antigen levels in the blood, Scan, etc.
Benign prostatic hyperplasia (BPH)
The prostate will almost certainly get larger increasing age. A small amount of prostate enlargement is present in many men over age 40 years of age. More than 90% of men over age 80 have the condition. It’s not clear why it happens, but it may be linked to the decline in the male sex hormone testosterone with aging. This enlargement is a condition called benign prostatic hyperplasia (BPH). The key word is benign. BPH has nothing to do with cancer and doesn’t increase the risk of prostate cancer. It can make urination and ejaculation difficult because as the prostate grows, it presses on the urethra. That interferes with the flow of urine and the release of ejaculate during orgasm. In less than half of all men with BPH, symptoms may include dribbling at the end of urinating, Inability to urinate (urinary retention), Incomplete emptying of the bladder, Incontinence, needing to urinate two or more times per night, Pain with urination or bloody urine (these may indicate infection). Slowed or delayed the start of the urinary stream, straining to urinate, Strong and sudden urge to urinate, and Weak urine stream.
The Link between BPH and Sexual Problems
Scientists aren’t sure why, but they agree that the worse the BPH symptoms are, the more likely an individual is to have sexual issues such as reduced sex drive, trouble keeping an erection, and less sexual satisfaction. It may have something to do with genetics or age. It’s also possible that the sleeplessness or anxiety that can come from an enlarged prostate makes sexual problems worse.
Laboratory Test for BPH.
A digital rectal exam is usually done to feel the prostate gland. Urine flow rate is monitored, Urinalysis to check for blood or infection, Urine culture to check for infection, Prostate-specific antigen (PSA) blood test to screen for prostate cancer, Cystoscopy, Blood urea nitrogen (BUN) and creatinine tests to check for reduced kidney function.
Risk Factors for BPH include;
- Age – symptoms start manifesting by age 50 to 60 in 60% of men.
- Unhealthy diet- daily consumption of a diet high in red or processed meat, saturated fats, and dairy products can increase your risk for prostate problems. Sodium (salt), Alcoholic and caffeinated beverages like coffee, tea, and soda can also increase your risk due to being diuretics that increase urine production.
- Type 2 diabetes, poorly managed Hypertension, and other heart diseases, Smoking, obesity, and a Sedentary lifestyle are common risk factors.
- Prostatitis
- Family history/genetics
- Frequent Urinary Tract infection (UTI)
Prostate Cancer
Cancer is a disease in which abnormal cells divide uncontrollably and destroy body tissue, in the case of prostate, abnormal prostate cells continue to grow until it has destroyed normal body tissues around and beyond the prostate. Prostate cancer usually develops slowly, so there may be no signs for many years. Symptoms of prostate cancer do not usually appear until the prostate is large enough to affect the tube that carries urine from the bladder out of the penis (urethra). When this happens, one may notice things like increased need to pee, straining while peeing, a feeling that the bladder has not fully emptied. Causes of prostate cancer are largely unknown. However, certain things can increase the risk of developing the condition.
Risk factors for Prostate cancer include;
- Age: The chances of developing prostate cancer increase as one gets older. Most cases develop in men aged 50 or older. Prostate cancer risk begins to rise sharply after age 55 years and peaks at age 70–74, after which it starts to decline. For reasons not yet understood, prostate cancer is more common in black men and less common in Asian men.
- Men whose fathers or brothers were affected by prostate cancer are at slightly increased risk themselves.
- Other risk factors include Obesity, Smoking (increases steroid hormone production such as DHT, and estrogen), High levels of pesticides, excessive consumption of dairy products (milk, yogurt, cheese, lactose-free milk, and fortified soy milk and yogurt), excessive red meat consumption, Saturated fat, and Sedentary lifestyle.
Beneficial Foods to Eat
A diet rich in fruits, vegetables, and healthy fats, such as the Mediterranean diet, may benefit health. Salmon, rich in healthy fats that contain omega-3 fatty acids, helps prevent and reduce inflammation within the body, and other cold-water fish, such as sardines and trout, are also rich in these fats.
Tomatoes: Tomatoes are packed with lycopene, an antioxidant that may benefit prostate gland cells. Cooking tomatoes, such as in tomato sauce or soup, helps to release the lycopene and make it more readily available to the body. Berries: Strawberries, blueberries, raspberries, and blackberries are excellent sources of antioxidants, which help to remove free radicals from the body. Free radicals are the byproducts of reactions that occur within the body and can cause damage and disease such as concern over time.
Broccoli: Broccoli and other cruciferous vegetables, including bok choy, cauliflower, Brussels sprouts, and cabbage, contain a chemical known as sulforaphane. This is thought to target cancer cells and promote a healthy prostate.
Nuts: Nuts are rich in zinc, a trace mineral. Zinc is found in high concentrations in the prostate and is thought to help balance testosterone and DHT. Besides nuts, shellfish and legumes are also high in zinc.
Citrus: Oranges, lemons, limes, and grapefruits are all high in vitamin C, which may help to protect the prostate gland.
All these are vital in addition to exercises to strengthen the pelvic floor muscles, such as brisk walking, Kegel exercise, and moderate strength training.
(Written by Ebenezer Dic-Ijiewere PhD.)
Our connections with family, friends, and colleagues are crucial. Individuals who have strong social connections and supportive relationships are more likely to adopt healthy lifestyles and effectively cope with stress, anxiety, and depression, especially during difficult times. A supportive network of family members, close friends, and colleagues provides a sense of belonging and emotional support.
Ways to create meaningful impacts are;
1.Showing kindness: Providing a listening ear, checking in on them, offering assistance, or simply sharing a smile can profoundly influence the overall well-being of others.

2. Promoting physical activity: Encouraging others to participate in physical activities such as organizing sports events, walking or running together, or engaging in group activities can enhance physical and social well-being.

3. Spreading awareness and education: Educating others about healthy lifestyle choices, including proper nutrition, exercise, and stress management, can empower them to make positive life changes.

4. Promoting a healthy diet: Sharing recipes, discussing healthy eating habits, organizing cooking classes, and advocating for nutritious foods can encourage healthier dietary choices.

5. Supporting access to healthcare: Being present for others during difficult times is crucial and can significantly improve their lives. Providing transportation to healthcare facilities encourages them to seek professional help when needed, and assisting with paperwork can make access easier.

6. Advocating for policy changes: Supporting policies and initiatives that promote public health, such as mental health services, water regulation, and access to healthcare, can have a broad impact on the well-being of entire communities.

7. Assisting those with chronic illnesses: Offering understanding and support to individuals with chronic health conditions can help them manage their conditions and enhance their quality of life.

 The Struggle to Survive: Living Through the Rising Cost
The Struggle to Survive: Living Through the Rising CostThe rising cost of living has become a significant public health concern, particularly for low-income individuals who are struggling daily to survive. Addressing the social determinants of health among this population remains an urgent issue, as many face ongoing challenges accessing essential needs such as food, housing, transportation, and healthcare. During my assessment of some of the low-income individuals, I found that several individuals eat only once a day to save money for rent. Many reported choosing to go hungry rather than risk homelessness. Some have been living in their cars for nearly a year, while others rely on the homes of friends to shower and change clothes. It is heartbreaking to witness the difficult situations people endure every day to stay alive.
The rising cost of living has multiple impacts on health and well-being. According to Grewal et al. (2024), increasing housing costs—one of the key components of living expenses—can have both direct and indirect health consequences. Their study indicates that:
- Financial strain from high housing and living expenses contributes to increased stress, anxiety, and depression, particularly among renters and low-income individuals.
- Food insecurity often results when households must prioritize rent or transportation over nutrition, leading to poor dietary intake and higher risks of chronic diseases.
- Limited access to healthcare arises when individuals cannot afford medical visits, medications, or preventive care due to competing financial demands.
- Housing instability or homelessness can expose individuals to unsafe environments, lack of sanitation, and interrupted social support networks, which worsen both physical and mental health outcomes.
Overall, Grewal et al. (2024) emphasize that the effects of rising housing and living costs are unequally distributed, disproportionately affecting low-income individuals who already face multiple barriers to health. This highlights the need for comprehensive policy approaches that integrate housing affordability, income support, and healthcare access as essential strategies to promote health equity.
Source: https://doi.org/10.1186/s12889-024-18360-w
 Unlocking the Benefits of Consistent Physical Activity
Unlocking the Benefits of Consistent Physical ActivityInadequate exercise or physical activity can contribute to the prevalence of non-communicable diseases. Given that non-communicable diseases account for over 80% of deaths in some nations, they are regarded as “the number one killer” globally. Physical exercise is any movement that requires energy, like housework, manual labor, walking, or manual labor. Exercise, on the other hand, is a regimen of physical activity that is organized and planned to enhance physical fitness.
Evidenced-based benefits.
- Physical Health: Research reported that 150 min of moderate-intensity or 75 min of vigorous-intensity physical activity led to a 14% risk reduction in all-cause mortality in patients with cardiovascular disease. In healthy adults, the risk decreased by 7%. Regular exercise has been shown in numerous studies to be beneficial in lowering the risk of cardiovascular disease as well as improving the health of patients with a variety of other conditions, such as certain cancers. stroke, type 2 diabetes, age-related sarcopenia, obesity, and multiple sclerosis.
- Mental Health: Research findings indicate that youth with mild to moderate mental health issues can benefit from organized sports and exercise programs. In one study, participants highlighted the significance of intensity choice for their enjoyment and commitment to the program, and it was shown that a self-selected intensity sport and exercise intervention was beneficial for depression. Research findings indicate that youth with mild to moderate mental health issues can benefit from organized sports and exercise programs. In one study, participants highlighted the significance of intensity choice for their enjoyment and commitment to the program, and it was shown that a self-selected intensity sport and exercise intervention was beneficial for depression. Also, engaging in physical exercise for 14 weeks can considerably improve mental symptoms, reduce anxiety and somatization, lessen obsessive-compulsive symptoms, and lift depressed moods.
- Quality Sleep: Study indicated that quality of sleep was positively impacted by exercise. Additionally, insomnia was somewhat alleviated following the exercise intervention. For instance, studies reveal that first-year students who exercise more get better sleep than those who exercise less during the night.
Evidenced-based research recommended the following:
- Adults should aim for more than 300 minutes of moderate-intensity aerobic physical activity, 150 minutes of vigorous-intensity aerobic physical activity spread out over the week, or an equivalent mix of moderate-intensity and vigorous-intensity aerobic physical activity.
- Engage in moderate-to-intense muscle-strengthening activities that target all major muscle groups two or more days a week.
- Adults 65 and older engage in multicomponent physical activity that involves functional balance and strength training at a moderate or higher intensity for at least three days a week in addition to aerobic exercises.
 Four lifestyle changes to reduce the development of Uterine Fibroids (UFs)
Four lifestyle changes to reduce the development of Uterine Fibroids (UFs)Uterine fibroids (UFs) are the most common benign tumors found in women of reproductive age, with a disproportionate impact on women of color. These disparities are believed to be combined with environmental, genetic, and socio-economic factors.
Some of the lifestyle changes that can help prevent or reduce the development of uterine fibroids are;
- Decreasing Alcohol consumption: It’s advised that women decrease their alcohol consumption to reduce the risk of developing uterine fibroids (UFs). Studies have reported an association between alcohol intake and an increased likelihood of UFs. Studies believe that alcohol may alter hormone levels and disrupt hormonal balance, contributing to the formation of UFs. It is advisable to consult with a healthcare professional for personalized advice based on unique health occurrences. By being mindful of alcohol consumption and adhering to recommended limits, proactive steps can be taken to lower the risk of UFs.
- Engage in at least four hours of vigorous physical activity per week: Research has found a significant association between an increased BMI and the risk of UFs. Obesity is believed to be a contributing factor to UF. Studies believe that women who engage in at least four hours of vigorous physical activity per week are more likely to encounter a decrease in the risk factors of UFs.
- Consuming more fruits, Vegetables, and dietary fibers: High intake of processed and refined foods, unhealthy fats, and sugary drinks, and low consumption of fruits, vegetables, and fiber-rich foods may contribute to hormonal imbalances, inflammation and oxidative stress, thereby encouraging the growth of UFs as indicated in the research. Additionally, a lack of fruits, vegetables, and fiber-rich foods has been reported to be associated with an elevated risk of UFs. Fruits, vegetables, and fiber-rich food are excellent sources of antioxidants, vitamins, and minerals that help combat oxidative stress and inflammation. Specifically, Dietary fiber has been indicated to have protective impacts against UFs by supporting hormonal balance and improving regular bowel movements. Hence, adopting a healthy and balanced diet with whole grains, fruits, vegetables, lean proteins, and healthy fats is essential.
- Managing stress: Studies have found that chronic psychological stress could increase the risk of uterine fibroids and indicated a significant link between chronic psychological stress and an elevated risk of UFs, predominantly among non-Hispanic Black women. Eating healthy, exercising regularly, getting enough sleep, relaxing, connecting with friends and family, and practicing mindfulness are some ways to manage stress.
 Strategies for Improving Sleep Quality
Strategies for Improving Sleep QualitySleep is essential for the health and well-being of children, adolescents, and adults. Quality sleep supports emotional well-being, metabolic health, cognitive function, mental health, and cardiovascular and cerebrovascular health. Additionally, getting sufficient, high-quality sleep helps reduce the risk of fatigue-related accidents and injuries, such as motor vehicle accidents and workplace incidents.
Recommended Sleep Duration
The American Academy of Sleep Medicine (AASM) and the Sleep Research Society (SRS) recommend that adults aim for at least 7 hours of sleep each night to promote optimal health. Similarly, the National Sleep Foundation (NSF) advises adults to get 7 to 9 hours of sleep per night, with older adults requiring 7 to 8 hours.
Prevalence of Sleep Disorders and Mental Health Impacts
About one-third of the population experiences insomnia symptoms, such as difficulty falling or staying asleep. Additionally, 4% to 26% of individuals report excessive sleepiness, and 2% to 4% have obstructive sleep apnea. Insomnia is associated with a significantly increased likelihood of mental health issues; individuals with insomnia are 10 times more likely to experience clinically significant depression and 17 times more likely to experience anxiety compared to those without insomnia. Poor sleep is also linked to post-traumatic stress, eating disorders, and psychosis spectrum experiences, such as delusions and hallucinations.
Improving sleep Quality
Improving sleep quality benefits mental health, and research reports that sleep plays a causal role in mental health challenges. Better sleep positively affects future mental health, even those without clinical symptoms.
Strategies for Improving Sleep Quality
- Creating a relaxing sleep environment
- Limiting daytime naps
- Managing stress and worries
- Being mindful of food and drink choices
- Sticking to a consistent sleep schedule
- Incorporating physical activity into daily routines.
 Coronary Heart Disease Risk Factors: Measures for Reduction
Coronary Heart Disease Risk Factors: Measures for ReductionCoronary Heart Disease (CHD) is a chronic and intricate ailment associated with substantial morbidity and mortality, primarily attributed to atherosclerotic lesions in coronary vessels, ultimately leading to myocardial infarction (MI) and stroke. Unhealthy eating habits, often influenced by chronic inflammation, are closely linked to CHD. Various health conditions, lifestyle choices, as well as your age and family history, can elevate the risk of developing heart disease; approximately 47% of Americans have at least one of the three primary risk factors for heart disease: high blood pressure, elevated cholesterol levels, and smoking. Certain risk factors for heart disease, such as age or family history, are beyond your control. However, you can proactively reduce your risk by changing the factors you can control.
Behaviors that heighten the risk for heart disease are
- Smoking: The Food & Drug Administration (FDA) estimates that cardiovascular disease causes 800,000 deaths and 400,000 premature deaths per year. About one-fifth and one-third of these result from smoking, respectively. Additionally, research reported that smoking resulted in a 51% increased risk of coronary heart disease in patients with diabetes. Cigarette smoking has the potential to harm the heart and blood vessels, amplifying the risk for heart conditions like atherosclerosis and heart attacks. Even nonsmokers face an increased risk of heart disease when exposed to secondhand smoke.
- Excessive alcohol consumption can elevate blood pressure and elevate the risk of heart disease. It also leads to increased triglyceride levels, a fatty substance in the blood associated with an elevated risk of heart disease.
- Sedentary lifestyle: Insufficient physical activity is a precursor to heart disease and can strengthen the likelihood of other medical conditions that serve as risk factors, including obesity, high blood pressure, high cholesterol, and diabetes. Engaging in regular physical activity can effectively decrease the risk of heart disease.
- Unhealthy Eating Habits: A diet rich in saturated fats, trans fats, and cholesterol has been associated with heart disease and related conditions like atherosclerosis. Recent research has provided more explicit evidence that trans-fat significantly raises the risk of cardiovascular disease by adversely affecting lipids, endothelial function, insulin resistance, and inflammation. For each 2% increase in calories consumed from trans-fat, there is a 23% higher risk of coronary artery disease. Recent studies and systematic reviews have focused on red and processed meat consumption. The research consistently demonstrates an increased risk of coronary heart disease and cardiovascular events. The risk ranges from 15% to 29% higher with red meat consumption and 23% to 42% higher with processed meat consumption
Measures for Reducing the Risk of Coronary Heart Disease
- Educating children and adolescents about the dangers of smoking to deter the initiation of tobacco use. The Food & Drug Administration (FDA) reported that the risk of coronary artery disease decreases to the level of lifetime nonsmokers within four years of quitting and within ten years.
- The DASH, Mediterranean, and vegetarian diets have the most evidence for cardiovascular disease prevention. The DASH diet has been shown to lower systolic blood pressure by up to 11.5 mmHg in adults with hypertension. Additionally, reported findings indicate a 21% reduction in coronary artery disease risk with adopting the DASH diet.
- The American Heart Association suggests substituting saturated fat with polyunsaturated and monounsaturated fats. A 5% shift from saturated fat to polyunsaturated fat consumption is linked to a 10% lower risk of coronary artery disease.
- Engaging in about 150 minutes per week of moderate-intensity aerobic activity significantly lowers the risk of cardiovascular disease. Moderate-intensity aerobic exercise is characterized by activity that maintains a heart rate between 50 to 70 percent of the individual’s maximum heart rate, calculated as 220 beats per minute minus the person’s age.